Malaria kills around half a million people per year, many of those children in developing countries. There are vaccines available, but they offer short-term protection to only around 30 percent of recipients.
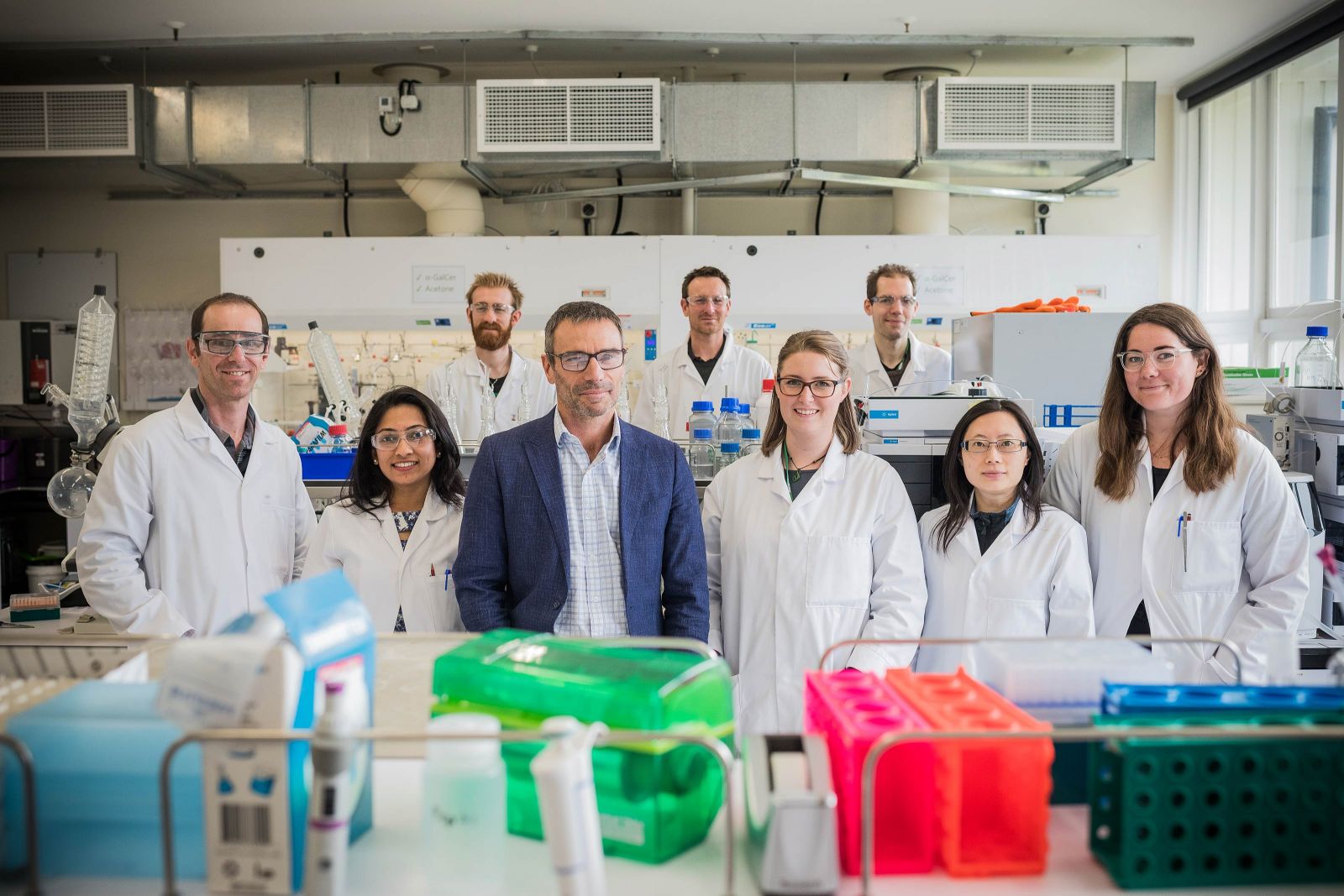
The University’s Ferrier Research Institute is part of a trans-Tasman collaboration aiming to change that with the development of a simple and effective vaccine that could be manufactured efficiently and administered easily in at-risk countries.
The research endeavour began three years ago, says Ferrier Research Institute Professor Gavin Painter.
“A number of things came together to put us on the path to a malaria vaccine,” says Gavin.
“Firstly, together with Professor Ian Hermans at the Malaghan Institute for Medical Research, we were—and still are—working on cancer vaccines that work by stimulating immune cells called T-cells, a type of white blood cell that is an essential part of the immune system. Knowing that T-cells are important in many other diseases, Avalia Immunotherapies, an immunology and drug development company spun out of the University, facilitated investigations into using this cancer vaccine concept for infectious diseases.”
As a result of this discovery, Gavin and his team began work with a University of Melbourne-based research team taking the first steps to develop a universal influenza vaccine.
“The ultimate goal of this research is to work with Avalia and Wellington UniVentures, the University’s commercialisation office, to commercialise this technology and have it out in the world, saving lives.”
This led to the Ferrier team connecting with multiple researchers, including another Melbourne-based team led by Professor William Heath that was interested in tackling malaria.
“From our earlier work it became clear our vaccines produced a specialised T-cell response in the liver—and this was what this group was looking for when it came to fighting malaria.”
With these initial successes on their side, Gavin and the trans-Tasman team began pivoting their current vaccines to target malaria.
“Excitingly, our first vaccines for malaria showed promise, and following further design and optimisation studies, we have some even better results,” Gavin says. “It is really hard to produce the right kind of T-cell response in the liver, but by working alongside Professor Heath and his team, who are malaria experts, we were able to combine our expertise and their knowledge to overcome this obstacle and produce some really exciting work.
“The ability to target specific tissues like the liver really sets this vaccine apart,” Gavin says. “This represents a fundamentally new way to think about how to design vaccines.”
The malaria vaccine project received nearly $1.2 million in funding from the Health Research Council of New Zealand this year that builds on previous funding from the Ministry of Business, Innovation and Employment and investment from Avalia. The funding will support Wellington- and Melbourne-based researchers to synthesise and test a series of vaccines to work out which malaria proteins (referred to as antigens) can be targeted by T-cells to stop infection.
The choice of antigen to target is important, as this is what the immune system ‘remembers’ if a vaccinated person is subsequently exposed to infection. As a result, T-cells are triggered to fight the disease, so the infection doesn’t take hold. Finding the most effective antigens is very important—especially for malaria where very few T-cell antigens have been defined. The new vaccines provide a new way to do this quickly.
The vaccines will be synthesised at the Ferrier Research Institute by scientist Sarah Draper, using a piece of equipment called a peptide synthesiser. The peptides made will be fragments of malaria antigens that, when injected into the body, ‘train’ T-cells so they can locate and destroy infected cells.
“We could not have done this research without Sarah, or without the peptide synthesiser,” Gavin says. “Our whole lab is based around this piece of equipment, and it is the only one at the University.
“The ultimate goal of this research is to work with Avalia and Wellington UniVentures, the University’s commercialisation office, to commercialise this technology and have it out in the world, saving lives,” Gavin says.