Chemical immunology
The immunoactive compounds we design and synthesise with the Malaghan Institute are being developed as novel treatments for cancer and allergic diseases.
Cancer immunotherapy
Working in partnership with the Malaghan Institute of Medical Research, we are designing cancer vaccines that help our own immune system reject a cancer. Current cancer drugs act by poisoning malignant tissue directly, but cancer vaccines offer a new approach. They are well tolerated by the body, have fewer side effects and may be more effective in the long term.
We have developed a cellular immunotherapy that is currently in clinical trials. A personalised vaccine is manufactured for each patient, made up of three parts—dendritic cells derived from a patient’s own blood, a chemical adjuvant and tumour antigens. Our role was to design and make the adjuvant, which is an immune stimulant.
Since these cellular therapies are time-consuming and expensive to make, a synthetic cancer vaccine was seen as a better approach that was capable of stimulating cancer rejection in a range of patients and was more easily manufactured,. This is an important focus of our ongoing work.
Collaborators
- Dr Ian Hermans, Malaghan Institute of Medical Research
- Dr Robert Weinkove, Capital and Coast District Health Board
- Prof Margaret Brimble, Peptide Synthesis Facility, University of Auckland
- Dr David Larsen, Chemistry Department, University of Otago
- GlycoSyn, Callaghan Innovation
- Dr Ben Greatrex, University of New England
Staff
Dr Gavin Painter is the programme lead.
Professor
Ferrier Research Institute
Senior Scientist
Ferrier Research Institute
Senior Scientist
Ferrier Research Institute
Research projects
Some cancer immunology projects are suitable for postgraduate research projects, including Masters and PhD theses. Please contact Dr Alison Daines for more information.
Senior Scientist · Postgraduate Coordinator
Ferrier Research Institute
Melanoma vaccine
We have created a cellular vaccine for melanoma in collaboration with the Malaghan Institute, the GMP Peptide Facility at the University of Auckland and GlycoSyn
The vaccine is currently being trialled in 46 subjects, with results expected in late 2016. All three parts, of the vaccine were manufactured under cGMP (Good Manufacturing Practice) in New Zealand:
- dendritic cells isolated from a patient’s blood were prepared at the Malaghan Institute
- tumour-associated antigens were synthesised at the GMP Peptide Facility
- the adjuvant was made by GlycoSyn using Ferrier’s synthesis and analysis methods.
Allergy and asthma vaccines
Work by our collaborators at the Malaghan Institute has shown that a cytotoxic T-lymphocyte response induced by a synthetic vaccine could be used to supress an allergic response. This is a unique way to use the immune system to fight allergy.
Reference
A self-adjuvanting vaccine induces cytotoxic T lymphocytes that suppress allergy. Nature Chemical Biology (2014)
Synthetic cancer vaccine
In the last three years we have developed a promising new synthetic cancer vaccine technology.
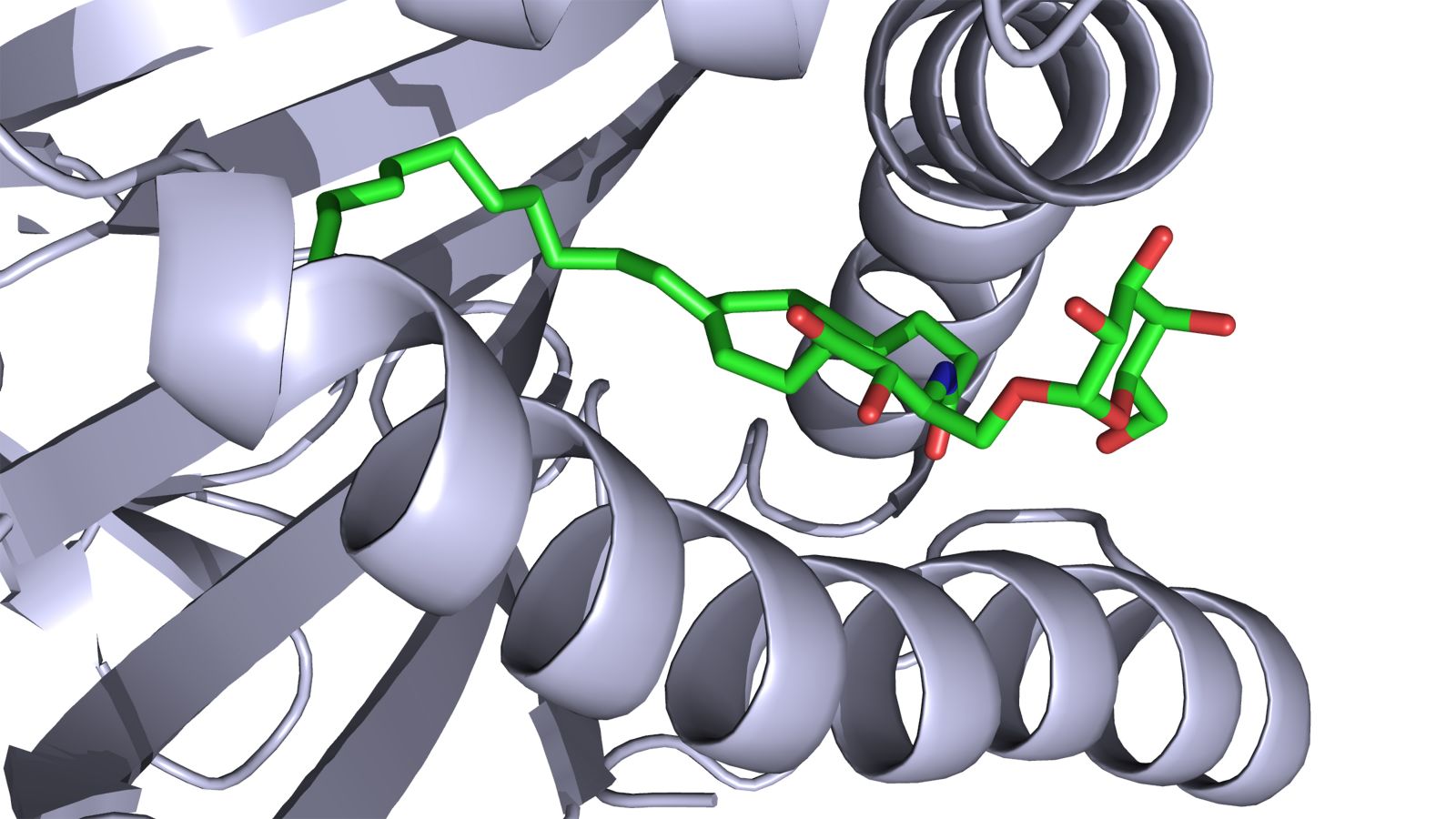
This technology chemically links a glycolipid (that can activate natural killer T cells) and a tumour-specific peptide antigen with a linker designed to allow the vaccine components to be selectively released inside the immune system’s professional antigen presenting cells.
In animal models, these synthetic vaccines elicit a very powerful immune response and produce huge numbers of cells that are highly targeted to the tumour cells. In a therapeutic model, where the cancer is established, we see tumour regression for a significant period of time.
The next step is to progress the technology to clinical trials.
Reference
An autologous leukemia cell vaccine prevents murine acute leukemia relapse after cytarabine treatment. Blood (2014)




